One out of ten people in the United States will develop peptic ulcer (PUD) disease sometime during their lifetime. Will you have peptic ulcer disease? How can you prevent it? What natural remedies help PUD?
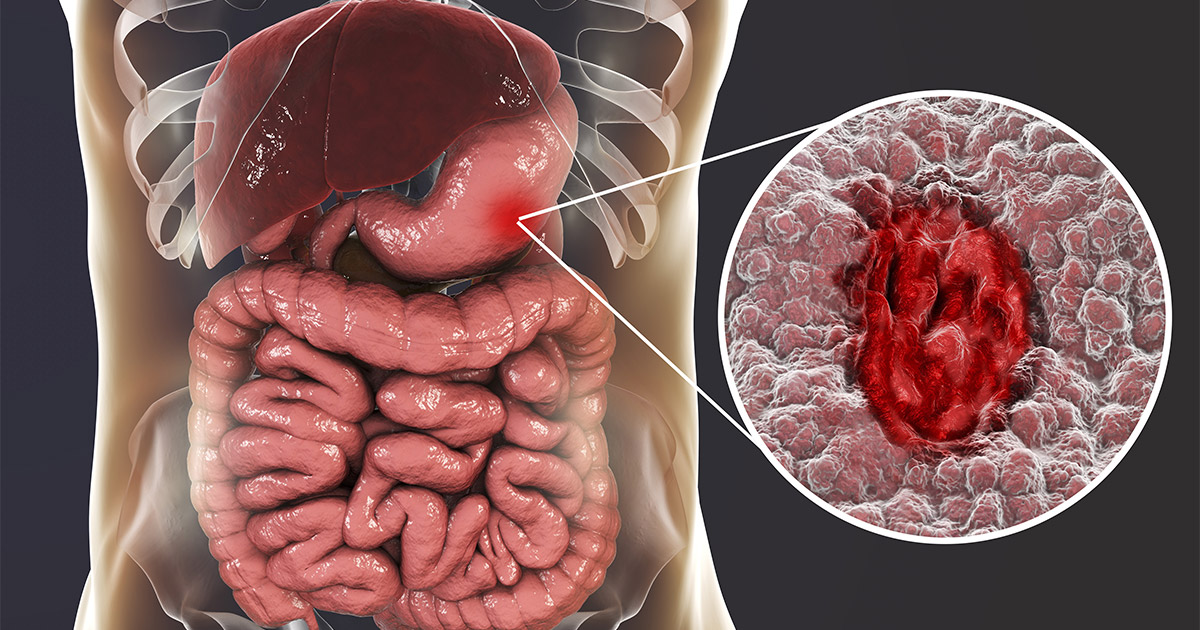
In the digestive system, an ulcer is an area where tissue has been destroyed by stomach acid, pepsin, or an infectious agent. This creates a sore, an open and painful wound in the mucosa. If not treated promptly, this damage can penetrate further into the muscular layer of the stomach or duodenum, producing bleeding, pain, and even perforation!
Peptic Ulcers 101
What exactly is this common but serious medical condition? What causes it, and what can be done to prevent or heal it? Depending on their location, peptic ulcers have different names: Gastric ulcers occur in your stomach. Duodenal ulcers develop in the first part of the small intestine (duodenum).
Signs and Symptoms
Pain from gastric ulcers can occur anytime during the day, especially immediately or within a few hours after eating. Pain arising from duodenal ulcers, the most common type, often occurs when the stomach is empty or during the night and can be temporarily relieved by food intake. However, approximately 20 percent of all peptic ulcer cases are asymptomatic.
Other signs and symptoms of PUD may include nausea and vomiting, belching, bloating, loss of appetite, and blood (often undetected by the naked eye) in the stools. Start with a good diagnostic workup. The signs and symptoms of PUD could indicated a more serious condition such as gastric cancer. GERDS, gastritis, pancreatitis, gallbladder problems, and occasionally a heart attack in women, may share some of the same symptoms. So getting an accurate diagnosis is critical.
Incidentally, the same nerves that innervate the esophagus also innervate the heart. An ECG may be necessarily to rule out cardiac problems. We highly recommend that indigestion, heartburn, and ulcers be thoroughly evaluated by a physician with diagnostic testing, such as upper gastrointestinal series (x-ray), ultrasound of the abdomen, endoscopy with biopsy, or gastric analysis if symptoms persist. Too many individuals suffer heart attacks after misinterpreting the warning signals as merely indigestion or an ulcer!
Risk Factors
The main cause of peptic ulcers is a stomach infection caused by a bacterium called Helicobacter pylori (H. pylori). Please note a high sodium diet can increase the risk of H. Pylori. Infections, the use of non-steroid anti-inflammatory drugs such as aspirin or ibuprofen, anxiety and depression are also contributing factors to peptic ulcers. Although lifestyle factors such as chronic stress, alcohol, smoking, and drinking coffee were long believed to be primary causes of ulcers, it is now thought that they only increase susceptibility to ulcers in some H. pylori carriers. Shift work and fragmented sleep may also increase one’s risk for PUD.
How about H. Pylori?
This dangerous spiral–shaped bacterium is a common cause of the infection worldwide. H. pylori infection is usually contracted in childhood; it may happen through food, water, or close contact with an infected individual. Most people with H. pylori don’t display any symptoms until they’re older. In fact, they may go through life unaware that they’re infected. Half of the world’s population has H pylori. Although H. pylori infection usually doesn’t cause problems in childhood, if left untreated it can cause chronic infection, gastritis (the irritation and inflammation of the lining of the stomach), peptic ulcer disease in 10% of cases, and even stomach cancer in 1%. It may be certain strains of these bacteria are more dangerous than others.1
H. pylori lives and multiplies within the mucous layer that covers and protects tissues that line the stomach and small intestine. Often, H. pylori causes no problems, but sometimes it can disrupt the mucous layer and inflame the lining of your stomach or duodenum, producing an ulcer. To cure H. pylori infection, physicians generally prescribe antibiotics and other drugs that block acid production and increase the bioavailability of antibodies in the gastric mucosa. Proton pump inhibitors also help to stabilize some antibiotics. However, concerns are rising with such conventional therapies in the light of emerging evidence that frequent use of antibiotics for H. pylori infections increases its resistance to antibiotics and damage to the kidneys.
Natural Remedies for H. Pylori
Fortunately, other alternative therapies with less risk of resistance are available. Researchers O’Mahoney and associates found that certain herbs can kill the H. pylori bacteria. Listed in order of their effectiveness from greatest to least, turmeric, cumin, ginger, borage, black caraway, oregano, and licorice were all found to exert anti H. pylori activity.2 In addition, turmeric, borage, and parsley were also known to inhibit the adherence of H. pylori to the stomach lining. Apigenin, a flavonoid in chamomile, has also been demonstrated in test tubes to inhibit the growth of H. pylori. In vitro studies have found that garlic, as well, can inhibit the growth of some antibiotic-resistant strains of H. pylori. Even though herbs may be the more desirable method of cure, they do not yet prove always effective in eradicating H. pylori.
Cautions about Natural Remedies for Ulcers
If a person does go on the herbal route, we would stress the need for re-evaluation following treatment. If the infection still persists after botanical agents have been wisely applied in conjunction with any other needed lifestyle measures, judicious use of antibiotics may prove helpful. Indeed, in certain cases the risk factors for stomach cancer may make antibiotics a necessity.
Note that probiotic supplementation such as that in lactobacillus- and bifidobacterium-containing yogurt can improve the antibiotic eradication rates of H. pylori in humans and/or decrease their adverse side effects. Probiotics also decrease mucosal inflammation, thus accelerating healing of the gastric mucosal barrier.3,4
NSAIDS
Ulcers induced by NSAIDs (nonsteroidal anti-inflammatory drugs) account for approximately 25 percent of all gastric ulcers. The overall lifetime risk for PUD in persons taking NSAIDs is around 20 percent greater than for those not using these drugs. This reflects a risk similar to those patients with H. pylori infection. People take NSAIDs to curb the pain arising from serious inflammation.
However, a well-balanced vegetarian diet, temperance in eating, abstaining from coffee and alcohol, moderate exercise, judicious use of hydrotherapy, and anti-inflammatory herbs, all reduce the inflammatory agents within our bodies without predisposing ourselves to PUD.5Turmeric not only combats inflammation in about 14 known ways but also protects from inflammation and helps to heal peptic ulcers. Ginger is another herb with broad anti-inflammatory properties. When used in moderate amounts, it may afford some protection from peptic ulcers.
More Attacks on Gastric Mucosa
In addition to H. pylori and NSAIDs, alcohol, vinegar, many spices, and excess bile salts can damage the gastric mucosal barrier as well. Deficiencies in vitamin A and trace elements of zinc and folic acid also predispose to mucosa damage. An excessive amount of salt encourages H. pylori growth in the stomach as well. Sleep deprivation can worsen the effect of the NSAIDs indomethacin-induced damage in the mucosa. Sleep deprivation also increases gastric acidity, histamine, and gastrin (a hormone that increases HCL production) and reduces blood flow to the mucosal barrier.6
Acute stress and fear can also prove damaging to a healthful stomach lining. Irregularity in meals and sleep can imbalance the autonomic nervous regulation of the stomach.
Excessive Acid Production
Excessive acid production is a contributing factor in approximately 50 percent of the duodenal ulcers. However, individuals with a normal or even low acid output can also develop gastric ulcers. Thus, individuals with frequent heartburn, epigastric pain, abdominal pain, acid indigestion, and other possible symptoms of an ulcer should be medically evaluated before downing antacids. Factors that can trigger the production of excessive amounts of hydrochloric acid include stress, intake of caffeine, meat preservatives, and excess calcium.
Healing the Gastric Mucosa by Diet
Although no one specific diet has been conclusively proven to heal ulcers, the following foods have been shown to exert healing effects on the gastric mucosal barrier:
Good Fats
Olives contain anti-ulcerogenic properties that help to both protect against and heal ulcers, as well as exert an anti-inflammatory effect. Olive oil inhibits H. pylori.7 Use only cold-pressed virgin olive oil in reasonable amounts on salads. Keep it stored in a dark place as exposure to light decreases its health-giving phytochemicals.
Anti-Gizzard Erosion Factor
Fresh avocados, cabbage and/or its juice, and other leafy salad greens contain the anti-gizzard erosion factor (sometimes called “Vitamin U”) that help heal ulcers—at least the ulcers in chicken gizzards. Since this phytochemical is sensitive to light, heat, and oxidation, the rule is—the fresher the better!
Healing Fruits and Veggies
Orange fruits and vegetables and other dark green leafy vegetables provide beta-carotene and other carotenoids. Once inside the body, beta-carotene is converted into vitamin A which is necessary for the health and repair of the epithelial tissue in the stomach. Note that carotenoids are actually better absorbed from cooked carrots!
Blueberries and plantains contain anti-ulcerogenic compounds that stimulate the production of mucus in the gastric mucosal barrier. Cranberry extract might prove helpful, as well as 8 pomegranates! 9 Resveratrol from red grapes and ellagic acid from strawberries inhibit H. pylori.10
Flavonoids should become your good friends! Two good sources of flavones are celery and parsley. Nitrates from vegetables such as spinach, beets, and lettuce are helpful. The salivary glands take the nitrates and convert them into nitrites. The stomach converts nitrites into nitric oxide, a molecule that improves blood flow in the mucosa.11 A diet rich in fiber, especially pectin, is associated with reduced rate of ulcers. One study showed that a high fiber diet reduces the recurrence rate of duodenal ulcers by half!
Don’t Forget the Psyche!
As previously mentioned, but worthy of further discussion, stress affects the gastrointestinal tract. Fear can decrease blood flow to the stomach, while anger causes the capillaries in the stomach to become engorged, more friable, and susceptible to bleeding. Chronic anxiety can increase acid production. The following true account from the 1950’s poignantly illustrates the critical role of emotional health and the power of forgiveness.
“Maria” was from a wealthy family in Europe. She had come to the United States many years ago and experienced two unfortunate marriages. Now her current marriage was in deep trouble, as well. A bleeding stomach ulcer brought her to Wildwood Lifestyle Center & Hospital. She did not want surgery.
With her physician’s help, she worked through the problems in her marriage, as well as many others. However even with all the treatments, counseling, and her own persistence, she was still no better physically and continued to bleed. “Maria,” her doctor said, “you have worked so hard on your problems. Is there anything else that might be troubling you?” “I can’t think of a single thing.” Her doctor was ready to schedule her for surgery when, in the middle of the night, she was urgently called to Maria’s room. Maria was pacing violently back and forth, hands clenched, hissing repeatedly, “I hate her! I hate her!”
“Maria, whom do you hate? Why?” Eventually she told her doctor what had happened. Her grandparents were members of European nobility. Their only son had had a child out of wedlock—Maria. What affection she did receive had been from her grandfather, who truly loved her. However, her grandmother openly resented and hated her. It had now been years since she had held any communication with either of her grandparents. That very night her grandmother had called, telling her, “Your grandfather has died. It is your fault. You killed him.”“I killed him? How?” “Because you left the faith of your family and espoused another religion!”
This last accusation put Maria in touch with her previously pent up hatred. When after much prayer and counsel she was able to forgive her grandmother and write her a gracious, loving letter, she stopped bleeding, and her ulcer healed completely. Forgiveness, not surgery, was the needed treatment.
Melatonin—a Biological Hero
Melatonin, a hormone, produced in the pineal gland and the walls of the gut, exerts a wide array of the beneficial effects. It exhibits highly protective action in the stomach and pancreas. It accelerates the healing of chronic gastric ulcers by increasing both microcirculation in the stomach and production of beneficial prostaglandins. Melatonin production is very helpful for both gastric and duodenal ulcers.12,13 Other researchers have found that melatonin helps to eradicate H. pylori without the use of antibiotics.14
Although melatonin peaks during puberty and then begins to decline, lifestyle factors can affect its production. Stress, caffeine, alcohol, tobacco, and bright lights at night decrease melatonin levels significantly. Physical exercise, natural sunlight during the day, darkness at night, sufficient intake of calcium, and wise calorie restriction all improve its production.
Exercise May Help Ulcers
A study of more than 11,000 men and women showed that active men had one-half to one-third the risk of developing a duodenal ulcer over a 20- year period when compared to their sedentary counterparts. Men who walked or ran at least 10 miles a week were 62 percent less likely to develop an ulcer than physically inactive study participants.15 Of course, moderate exercise is the best type. Intense activity tends to draw too much blood away from the lining of the stomach and the intestines, thereby rendering the mucosa more susceptible to ulcer formation.
Herbal Helps for Ulcers
Numerous studies have found the anti-inflammatory herb licorice to be an effective anti-ulcer compound.16 Note, though, that glycyrrhizic acid, one of the primary active ingredients in licorice, can cause an elevation in blood pressure and in some individuals, salt retention, leading to rapid weight gain. Deglycyrrhizinated licorice (DGL) is a form of the herb with the glycyrrhizic acid removed. Studies show it may be a successful anti-peptic ulcer agent without any known side effects.17
Aloe Vera inhibits H. pylori. The gel of this succulent herb serves as a moisturizing emollient that promotes healing and stimulates protein synthesis in tissues.18 Please, note that individuals with low thyroid levels should not take aloe vera internally on a regular basis.
A few more words about ginger. In his book, The Green Pharmacy, medical botanist, James Duke, mentions that ginger contains 11 anti-ulcer compounds. Both it and the herb chamomile are purported to be helpful in treating ulcers.19 Many naturopathic-oriented doctors recommend drinking two to three cups of strong chamomile tea each day for treatment of PUD.
A cautionary note: if you are taking any medications, be sure to consult with your pharmacist regarding any potential herb-drug interactions before using botanical agents.
Complications from Ulcers
Complications from ulcers are not to be minimized. For one thing, they can lead to serious complications, such as:
Penetration: an ulcer eventually can eat entirely through the muscular wall of the stomach or duodenum and even into an adjacent organ! Possible signs would include piercing, persistent pain which may be felt elsewhere than the actual area involved. For example, the back may hurt when a duodenal ulcer penetrates the pancreas.
Perforation: an ulcer can erode a hole through the stomach wall, thus creating an opening into the abdomen.
Bleeding: much of the time this occurs in what is called occult (invisible to the eye) blood found in the stool. Because it is not readily seen, the inexpensive and simple test for occult blood is well-warranted. Some individuals also show symptoms of internal bleeding by vomiting what is termed coffee ground emesis which is dried blood from the stomach or GI tract.
Obstruction: swelling of inflamed tissues around an ulcer or scarring from a previous one can narrow the outlet from the stomach or slender duodenum, constituting a medical emergency.
Conclusions
In summary, peptic ulcers are serious, potentially costly, and can prove deadly. Anyone experiencing the symptoms of a peptic ulcer should have a thorough medical workup promptly. Cultivation of a healthful lifestyle and the elimination of unhealthful ones can both reduce risk for developing peptic ulcers and facilitate their healing. Peptic ulcer disease will often respond well to lifestyle medicine focusing on select natural herbal agents, a balanced diet, a faithful exercise program, and a trusting relationship with God. If ulcer symptoms persists after treatment, please see a doctor.
Disclaimer: The information in this article is general and educational in nature. Wildwood Sanitarium, its entities, or authors do not intend this information as a substitute for proper diagnosis, treatment, or counseling from a qualified medical provider who knows the person’s medical history and laboratory work.
Copyright © by Wildwood Sanitarium, Inc. 2026
References:
- University of Gothenburg. “Peptic Ulcer Bacterium Alters The Body’s Defense System.” ScienceDaily. ScienceDaily, 1 July 2009. https://www.sciencedaily.com/releases/2009/06/090629112825[↩]
- O’Mahony R, et. al, Bactericidal and anti-adhesive properties of culinary and medicinal plants against Helicobacter pylori, World J Gastroenterol, 11(47):7499, 507, 2005. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4725184/[↩]
- Gotteland M, et al, Systematic review: are probiotics useful in controlling gastric colonization by Helicobacter pylori? Aliment Pharmacol Ther, 15; 23(8):1077, 86, 2006, review. [↩]
- Sheu, B.S., et al, Pretreatment with Lactobacillus and Bifidobacterium containing yogurt can improve the efficacy of quadruple therapy in eradicating residual Helicobacter pylori infection after failed triple therapy. Am J Clin Nutr, 83(4):864, 9, 2006.[↩]
- Hall, Elizabeth, Proven Strategies to Defeat Inflammation. March 12, 2020. https://wildwoodhealth.com/blog/proven-strategies-to-defeat-inflammation/[↩]
- Jin, S. G., et al, Partial sleep deprivation compromises gastric mucosa integrity in rats. Life Science, 77(2):220, 229, 20058. [↩]
- American Chemical Society. “New Potential Health Benefit Of Olive Oil For Peptic Ulcer Disease.” ScienceDaily. ScienceDaily, 14 February 2007. https://www.sciencedaily.com/releases/2007/02/070212101701.htm[↩]
- Chatterjee A, et al., Inhibition of Helicobacter pylori in vitro by various berry extracts, with enhanced susceptibility to clarithromycin, Mol Cell Biochem, 265(1, 2):19, 26, 2004. [↩]
- Ajaikumar, K., et al, The inhibition of gastric mucosal injury by Punicagranatum L. (pomegranate) methanolic extract. J Ethnopharmacol, 96 (1-2):171-6, 2005. [↩]
- Antibacterial Effects of Grape Extracts on Helicobacter pylori. Applied and Environmental Microbiology, 2008; 75 (3): 848 DOI: 10.1128/AEM.01595-08. www.sciencedaily.com/releases/2008/05/080507105601.htm[↩]
- Uppsala University. “Nitrates In Vegetables Protect Against Gastric Ulcers, Study Shows.” ScienceDaily. ScienceDaily, 9 May 2008. [↩]
- Bandyopadhyay, D., et al., Melatonin protects against gastric ulceration and increases the efficacy of ranitidine and omeprazole in reducing gastric cancer. J Pineal Res, 33(1):1-7, 2002. [↩]
- Komarov, F., et. al, Melatonin production in patients with duodenal ulcer at different stages of disease. Klin Med (Mosk), 76(3):15, 8, 1998, Russian. [↩]
- Malinovskaya, N., et al., Anti-helicobacter effects of melatonin. Klin Med (Mosk), 85(3):40, 3, 2007.[↩]
- Yiling, C., et al., Does physical activity reduce the risk of developing peptic ulcers? Br J Sports Med, 34:116, 121, 2000. 11. Hall, E., Aloe Vera. J Health & Healing, 27(1):15, 2006.[↩]
- Momeni A. Effect of licorice versus bismuth on eradication of Helicobacter pylori in patients with peptic ulcer disease. Pharmacognosy Res. 2014 Oct-Dec; 6(4): 341–344.[↩]
- Murray M. DGL for Peptic Ulcers. https://doctormurray.com/dgl-for-peptic-ulcers/[↩]
- Hall, E., Aloe Vera. J Health & Healing, 27(1):15, 2006[↩]
- OgharA. Et al.,Assessment of some Herbal Drugs for Prophylaxis of Peptic Ulcer. Iran J Pharm Res. 2014 Summer; 13(3): 1081–1086.[↩]