More than 80% of people will suffer from back discomfort at some point in their lives. The annual cost in the United States for treating back pain has reached an astronomical $85 billion dollars! Low back pain (LBP) is the main cause of disability in the United States with more than 1 in 5 adults experiencing chronic pain.
Low back pain and dysfunction is the #1 musculoskeletal issue in the United States today. The total cost of treating back pain has jumped 65% in just the past decade. Unfortunately, after all the costly treatments offered them by modern medicine, many people are still left with an aching back and a deepening hole in their wallets.
This epidemic has placed physical therapists in a very unique position. As more people are looking for more economic and healthful ways to manage their back problems, the physical therapy profession offers very cost-effective methods of managing back problems and maximizing functional independence, with a minimum of pharmaceutical and surgical intervention
The Anatomy of Spinal Problems
The spinal column is divided into four different regions: the cervical, thoracic, lumbar, and sacral regions. Its most important function is to protect the spinal cord. It is also one of the most amazing and efficient stabilizing and shock-absorbing systems in nature. When the four curves of the human spine are in proper alignment, basic physics tells us that it can take 10 times more loading capacity. The majority of back and neck problems treated by the average physician, physical therapist, or chiropractor are directly related to three basic components: poor posture, poor body mechanics, and weak core muscles. It is therefore imperative that patients be thoroughly educated, instructed, and trained in these three areas in order for them to achieve optimum back health, slow down the wear and tear of aging, and prevent more severe injury.
Sources of Pain
Pain begins in the low back region for several reasons. There are pain receptors in the ligaments, muscles, facet joints, sacroiliac joints, intervertebral discs, peripheral nerve roots, the vertebral bodies, blood vessels, and the spinal cord. Ligaments, which are made up of collagen and elastin, are designed to support and stabilize the spine. When ligaments get stretched, the pain receptors get disrupted and create pain. If this stretching continues, the spinal column becomes unstable.
Diabetes and Back Pain
T2D is strongly linked with fractured vertebrae, intervertebral disc (IVD) degeneration, and severe chronic spinal pain. In type 2 diabetes, there is reduced blood flow to the skeletal muscles, greater muscle inflammation and calcified tendons, and damaged nerves supplying the muscles.1 A large study considered the risk of type 2 diabetes. In this study, there were enrolled 479,680 diabetes and 479,680 age- and sex-matched control subjects.The researchers found that type 2 diabetes was strongly associated with lumbar spine disorders and frequent spinal procedures.2 Other studies have indicated that chronic back pain (CBP) is more prevalent in patients with diabetes.3
Back Pain Doesn’t Always Originate from the Back
Trauma from motor vehicle or work-related accidents are increasingly common. There are also many diseases including cancer, multiple sclerosis, ALS, and shingles, along with visceral problems like kidney stones, colitis/ileitis, gallstones, and even cardiac conditions, all of which can contribute to varying degrees of back pain. The most common underlying cause of back pain is undoubtedly related to poor posture, deconditioning, and poor body mechanics (i.e. improper lifting techniques). Spinal stenosis, arthritis, scoliosis, osteoporosis, and compression fractures are also causes.
Referred Back Pain
Shoulder pain could radiate from the lungs, liver, or heart. A ruptured spleen could also cause upper back pain especially if it is between the shoulders. Lower back or flank pain may result from a problem with the kidneys or colon.
Contributors to Back Pain
The most important lifestyle issues leading to back pain are excess weight, improper lifting, dehydration, chronic fatigue, or a lack of proper rest (sleep disorders have also reached epidemic proportions), and a lack of regular, back-specific exercise. It is therefore very important before treating back pain to determine the underlying causes. Stress, anxiety, and depression increases the risk of spinal pain.4
Up In Smoke!
Smoking reduces blood flow to the spine. A large cohort study of over 438,000 participants linked cigarette smoking to back pain.Smoking is also strongly linked to osteoporosis and damages the microarchitecture of bone, including the vertebrae. The more a person smoked, the greater the risk of back pain. Reducing the number of cigarettes smoked and quitting smoking reduce back pain.5
Eat for Strength
Ample intake of protein reduces the risk of low back pain after adjusting for variables (age, sex, smoking, drinking, diabetes, physical activity, body mass index, and waist circumference). A review study has recently indicated that adherence to the Mediterranean and plant-based diet effectively reduces musculoskeletal pain.6
An observational study of 4,123 participants found that higher fruit, whole grain, and dairy intake were associated with 20% to 26% lower likelihood of chronic spinal pain. Added sugars were associated with 49% increased odds of chronic spinal pain.7 A Western style diet (high in animal products, refined carbs, saturated and trans fat, salt, low in fiber and whole plant foods) is linked to significant high levels of several pro-inflammatory agents and markers.8 An unhealthful, plant-based diet that incorporates large amounts of sugar, refined products, and which has inadequate B12, calcium, vitamin D can accelerate spinal osteoporosis.
Treatment for Back Pain
Once a complete evaluation and differential diagnosis has determined the primary source and cause of pain, then an appropriate treatment and plan of care can be implemented. This fact cannot be overemphasized, for if not properly evaluated, then it will never be properly treated, and will inevitably lead to chronic or more severe problems. This is one of the main reasons why pain often becomes a vicious, downward cycle which can lead to depression, disability, chemical addiction, and even death or suicide.
When the average person goes to his primary care physician (PCP) with a complaint of back pain, he will usually be prescribed a combination of medications: analgesics for pain, NSAIDS for inflammation, and muscle relaxers. In some cases herbal anti-inflammatories help. Approximately 80% of acute, non-traumatic back pain episodes will completely or significantly subside within 1-2 weeks, with or without medication. Ice packs applied for 20 minutes can ease acute inflammation whereas heat applied to the muscle spasms bring relief. It is better to keep heat off the spine if there is a suspected disc problem.
Physical Therapy
If the pain is chronic, or the acute phase does not resolve, then the PCP should refer that individual to physical therapy (PT). In most cases, physical therapy is extremely effective in relieving the pain and restoring normal mobility and function. Spinal decompression, TENS units, and other modalities often help.
In the approximately 10% that do not fully recover with PT, they may be referred to an orthopedic or neurosurgeon for further assessment and treatments, which may eventually need some type of surgical procedure to correct a more seriously damaged disc or compromised nerve.
Manipulations
Another popular form of back pain treatment is chiropractics which in most cases can provide significant pain relief and restoration of function. Massage therapy is another increasingly popular treatment that can be very effective in relieving muscle and soft-tissue pain.
There are a number of other treatment forms used in treating back pain, many of which fall under the category of non-biblical, new age healing. It has been my experience that most of these forms of “healing” are not very effective in the long term, neither are the methods reproducible or supported by well-established, sound, scientific methods. In addition, these approaches to healing can lead even an intelligent mind down a very dangerous path, to eventually accepting false science, theories, and doctrines.
Physical therapy has an amazing arsenal of non-invasive, proven, natural science-based modalities, procedures, and manual techniques used to effectively treat and prevent back pain. The initial evaluation and almost every subsequent treatment should involve educating the patient in proper posture, body mechanics, and a written home treatment and exercise program. The initial phase of treatment will usually focus on reducing the (acute) inflammatory stage of the injury or pain. This may include something as simple as the frequent application of cryotherapy (ice) and neutral resting postures, to the use of electrical stimulation and ultrasound for trigger points and muscle spasms, to various manual techniques for soft tissue and joint mobilization, and gentle therapeutic exercises, all to facilitate tissue healing.
The next (sub acute) phase may involve more progressive exercises to restore full range of motion. It will begin strength and low-impact aerobic training with less emphasis on modalities. The later phase of therapy should usually address upper-level strength and conditioning exercises, restoring the individual to full function.
In most cases, a simple 15-minute back workout can help people keep the muscles that support their back strong and flexible and their spines in better alignment.
To exercise safely, keep in mind several tips:
1. Check with your healthcare provider before starting an exercise program.
2. Expect some soreness at first. If pain worsens, stop the exercise and check with your healthcare provider.
3. Pace yourself. Start slowly and work up gradually to more vigorous exercise.
4. Stretch slowly. Don’t jerk or bounce.
5. Breathe slowly and deeply. Don’t hold your breath.
In summary, remember that a healthy back is a precious, amazing gift that can provide you with a lifetime of faithful service, if you are willing to invest a small amount of time learning and applying some simple exercises on a regular basis. Become more aware throughout the day of maintaining proper posture and body mechanics.
The 15-Minute Back Workout
Bridging
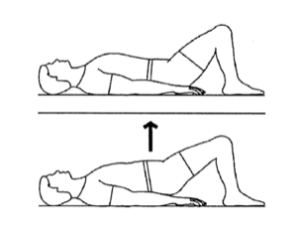
Lie on back with knees bent.
Lift buttocks off floor.
Return to start position.
Special Instructions:
Maintain neutral spine
Perform 3 sets of 10 repetitions, once a day.
Rest 1 minute between sets.
Perform 1 repetition every 4 seconds.
Prone elbow press up
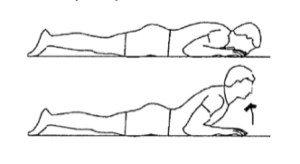
Lie face down, elbows bent, hands beside face.
Push up to elbows, keeping hips on floor.
Return to start position and repeat.
Special Instructions:
Perform at rate of one arch per second.
Progress by straightening arms, pushing up.
Perform 3 sets of 10 repetitions, once a day.
Rest 1 minute between sets.
Perform 1 repetition every 4 seconds.
Supine knee side-to-side
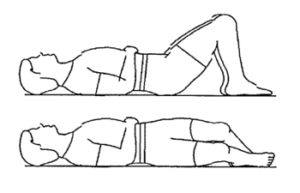
Lie on back with knees bent, feet flat on floor as shown.
Keeping knees together, move knees to the left as far as is comfortable.
Next, move knees to the right as far as comfortable.
Return to start position.
Special Instructions:
Keep your shoulders flat against the floor.
Perform 3 sets of 10 repetitions, once a day.
Rest 1 minute between sets.
Perform 1 repetition every 4 seconds.
Partial wall slide
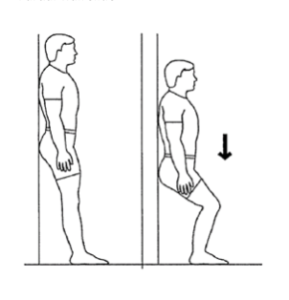
Lean on wall, feet approximately 12 inches from wall, shoulder distance apart.
Bend knees to 45 degrees.
Hold 5 seconds.
Return to starting position.
Special Instructions:
Perform 3 sets of 10 repetitions, once a day.
Rest 1 minute between sets.
Perform 1 repetition every 4 seconds.
Cat camel combo
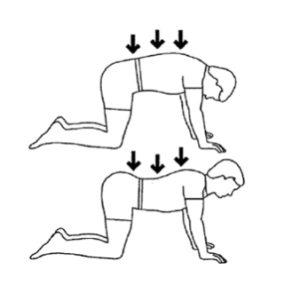
Begin in 4-point kneeling, back in neutral position.
Tuck chin in and continue by rounding back upward one segment at a time.
Reverse by letting back arch one segment at a time, but keep neck in neutral at the end.
Special Instructions:
Perform 3 sets of 10 repetitions, once a day.
Rest 1 minute between sets.
Perform 1 repetition every 4 seconds.
Kick-up hamstring stretch
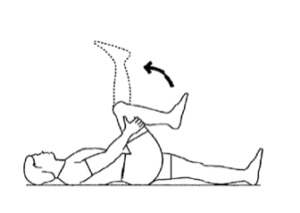
Lie on back holding knee from behind, pulled toward chest, as shown.
Gently straighten leg.
Repeat with other leg.
Special Instructions:
Perform 1 set of 5 repetitions, twice a day.
Hold exercise for 20 seconds.
© 2024, Wildwood Sanitarium. All rights reserved.
Disclaimer: The information in this article is educational and general in nature. Neither Wildwood Lifestyle Center, its entities, nor author intend this article as a substitute for medical diagnosis, counsel, or treatment by a qualified health professional.
Sources
- Wyatt LH, Ferrance RJ. The musculoskeletal effects of diabetes mellitus. J Can Chiropr Assoc. 2006 Mar;50(1):43-50. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1839979/↩
- Park, CH., Min, KB., Min, JY. et al. Strong association of type 2 diabetes with degenerative lumbar spine disorders. Sci Rep 11, 16472 (2021). https://doi.org/10.1038/s41598-021-95626-y↩
- Eivazi M, Abadi L. Low back pain in diabetes mellitus and importance of preventive approach. Health Promot Perspect. 2012 Jul 1;2(1):80-8. doi: 10.5681/hpp.2012.010.↩
- Linton SJ. A review of psychological risk factors in back and neck pain. Spine (Phila Pa 1976). 2000 May 1;25(9):1148-56. http://10.1097/00007632-200005010-00017 ↩
- Xu HR, et al. Association between smoking and incident back pain: A prospective cohort study with 438 510 participants. J Glob Health. 2023 Nov 22;13:04152. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10663706/ ↩
- Mendonça CR, Noll M, Castro MCR, Silveira EA. Effects of nutritional interventions in the control of musculoskeletal pain: an integrative review. Nutrients. 2020;12(10):3075. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7601187/↩
- Zick SM, Murphy SL, Colacino J. Association of chronic spinal pain with diet quality. Pain Rep. 2020 Aug 11;5(5):e837. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7431251/#R20 ↩
- Pasdar Y, Hamzeh B, Karimi S, Moradi S, Cheshmeh S, Shamsi MB, Najafi F. Major dietary patterns in relation to chronic low back pain; a cross-sectional study from RaNCD cohort. Nutr J. 2022 May 12;21(1):28. doi: 10.1186/s12937-022-00780-2↩

