Regarding lab testing for atherosclerosis or heart disease, it is not wise to only gauge one’s risk based on LDL and HDL cholesterol numbers. The particle size of LDL cholesterol counts too. Small dense LDLs are the most atherogenic. Higher numbers for HDL are beneficial only if the HDL is functional. Dysfunctional HDL encourages atherosclerosis. In this blog, you will learn the multifaceted contributions of HDL, if you are at risk of having dysfunctional HDL, and how to improve HDL function.
Nearly half of the people who get heart attacks have healthy cholesterol levels. Up to 65% of cardiovascular deaths cannot be prevented by assumed or supposed LDL-C lowering agents.1 Multiple clinical studies have identified individuals with a significant coronary artery disease despite normal or elevated levels of HDL. Conversely, some populations with very low levels of HDL-C have paradoxically lower rates of heart disease.2 Why?
Some Cholesterol is Good
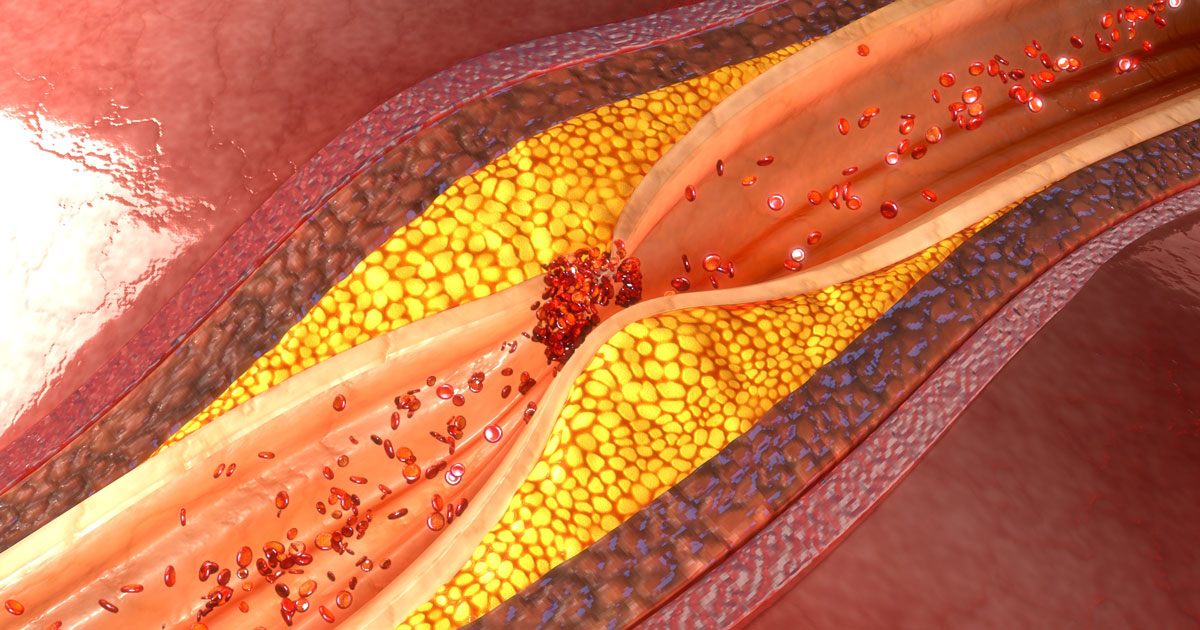
Your body needs a certain amount of cholesterol for the cell membranes, nerve insulation, and steroid hormones (sex hormones, cortisol, and vitamin D hormone). In fact, it makes all you need. You just don’t want it to clog your arteries or suppress your immune system as it becomes oxidized. Since cholesterol cannot dissolve in water, it is carried by trucks known as lipoproteins in the blood. Low-density lipoproteins (LDLs) take cholesterol to the cells and blood vessels. We need a certain amount of LDLs. An elevated LDL level, however, is a risk factor for coronary artery disease. HDLs (high density lipoproteins), as little trucks, transport cholesterol from your arteries to your liver. Put simply, HDL fights the “bad” cholesterol. HDL is a family; some members protect from bad cholesterol, whereas others do not. HDL-C is protective against heart disease under certain circumstances.
HDL Contributions:
High-density lipoproteins are super heroes, right? After all, HDLs defend the arteries from cholesterol build up.
- They act as cholesterol scavengers, pull cholesterol out of arteries, and carry cholesterol to the liver where it is converted into bile.
- HDLs exert anti-inflammatory activity.3 (Inflammation plays a major role in atherosclerosis.)
- HDLs also protect the innermost lining (endothelium) of arteries and reduce the risk of undesirable clot formation.4
- They stimulate the production of nitric oxide.5 In moderation, nitric oxide improves the ability of blood vessels to dilate.
- HDLs protect from free radical damage. Normal HDL helps to reduce oxidation of cholesterol. Oxidized cholesterol is toxic to the lining inside the arteries and suppresses the immune system.
Know Your Numbers, But Don’t Get Fooled
According to the Mayo Clinic your “good” cholesterol (HDL) should be 40 to 49 mg/dL if you are a man and 50 to 59 mg/dL if you are a woman, above 60 is ideal for HDL. A low HDL is considered as under 40 milligrams per deciliter of blood (mg/dL). High levels of HDL are generally associated with lower risks for stroke and heart disease whereas lower levels are associated with a substantial increased risk. As mentioned in our first paragraph, this might not always be true. In fact, just measuring the HDL-C level is probably not a good predictor of its cardiovascular benefits. Methods to evaluate HDL functions are required.6,7,8 Hold tight because in a few minutes we will address the lifestyle factors and medical conditions that can turn your good HDLs into dysfunctional HDLs.
Lifestyle Factors That Increase HDL:
- Stop smoking. Quitting smoking can increase your HDL cholesterol by up to 10 percent.9
- Weight loss (if obese). For every 6 pounds (2.7 kilograms) you lose, your HDL may increase by 1 mg/dL (0.03 mmol/L).10
- Regular or frequent aerobic exercise can increase HDL cholesterol by about 5 percent in otherwise healthy, sedentary adults.11
- Garlic, onions, and chromium help increase HDL.
- Monounsaturated and polyunsaturated fats — found in olive, peanut, and canola oils — tend to improve HDL’s anti-inflammatory abilities.
Please note: Inflammation is involved in all the developmental stages of atherosclerosis. Just reducing elevated LDL cholesterol levels without reducing the inflammation is not going to get at the problem sufficiently. Inflammation must also be confronted. Fortunately, many of the same lifestyle strategies that reduce cholesterol also exert a beneficial anti-inflammatory effect. One caveat though: No vitamin pill can replace the thousands of antioxidants and anti-inflammatory compounds found in plant foods!
Good Guys Turned Into Villains
The quality of HDL can be compromised. Unfortunately, under some conditions HDLs become dysfunctional and can actually promote atherosclerosis instead of protecting the arteries from it.12
Oxidized cholesterol pushes inflammation inside the arteries and encourages the development of atherosclerosis. Even though HDL is considered protective against atherosclerosis, HDL itself can become oxidized from smoking, a deficient diet, or a pro-inflammatory condition such as obesity, pre-diabetes, and diabetes. When HDL becomes oxidized, it becomes dysfunctional and cannot remove cholesterol from arteries. It loses its ability to protect cholesterol from oxidation. Dysfunctional HDL-C does not promote heart and blood vessel health even if HDL-C is present in high levels.13
Dysfunctional HDLs, especially when coupled with oxidized LDL, accelerate the development of atherosclerosis. This duo also increases the risk for undesirable clot formation. As we will soon see, a person’s diet and medical history should be carefully evaluated even when the cholesterol numbers are within normal levels.
What Causes HDL to Turn Bad?
Diabetes
In both metabolic syndrome and diabetes mellitus, the HDL particles undergo diverse structural modifications that change its function.14
Inflammation
Inflammation from influenza, infections, and other diseases can change and profoundly transform athero-protective HDLs to pro-atherogenic HDLs.15,16
Lipid Peroxides
The lipid classification includes fats, cholesterol, and phosphor-lipids. Free radicals damage fats. When fats are oxidized, they produce lipid peroxides and more free radicals that alter HDL function.17
One way to reduce this lipid peroxidation is to use cold-pressed, virgin, vegetable oils rather than regular commercial oil. The more an oil is heated, the more lipid peroxides are produced. Oxidation attacks the double bonds of fats, so monounsaturated fats like oleic acid in olives and plant-based omega-3 fats are superior to fish oil, for most people, because they have only one double bond.18 Fat-soluble antioxidants also help to reduce lipid peroxides.
Cigarette Smoking
Not only does smoking lower the HDL level, it can strip the protective portions of HDL. LCAT is an enzyme that is crucial for the maintenance of normal HDL metabolism. Smoking decreases LCAT. Smoking also encourages lipid peroxidation.19
Intake of Fats
Consumption of saturated fats reduces the anti-inflammatory potential of HDL and impairs the ability of blood vessels to dilate. In contrast, the anti-inflammatory activity of HDL improves after consumption of polyunsaturated fat.20
Medical Conditions
Besides pre-diabetes and diabetes, other medical conditions can convert our HDL superheroes into HDL villains. Certain autommune conditions: lupus erythematosus, rheumatoid arthritis, scleroderma can change the anti-inflammatory HDL into a pro-inflammatory HDL.21 Obstructive sleep apnea can also contribute to HDL dysfunction.
Elevated Homocysteine Levels
A high meat diet, deficiency in B12 and folic acid, low thyroid hormone, and kidney disease can elevate homocysteine levels. An elevated homocysteine level promotes both dysfunctional HDL and pushes inflammation inside the artery. 22
Environmental Pollutants
Breathing motor vehicle emissions triggers a change in high-density lipoprotein (HDL) cholesterol, altering its cardiovascular protective qualities so that it actually contributes to clogged arteries.23
How to Improve HDL Functionality:
Get sufficient good quality of sleep.
Get enough sleep by going to bed early. Why? “Night owls,” or individuals who prefer to be active during the night or early morning, have significantly higher levels of total cholesterol, triglyceride, and low-density lipoprotein cholesterol when compared with individuals who are larks (morning preference) after adjusting for confounding variables.24 Sleep deprivation decreases HDL and its functionality. If you have sleep apnea, there are several treatment options that can help you.
Engage in aerobic exercise every day.
Moderate exercise increases both HDL quality and functionality. When controlling for exercise patterns, diet, and sleep, moderate‐intensity exercise improved HDL function, lipid/lipoprotein profile, fitness, and body composition.25 15-minute walks after meals help to reduce blood glucose levels. Even in heart failure patients, a 15-week exercise program improved HDL functionality.26
Lose weight if obese and improve blood glucose level.
In individuals who have the metabolic syndrome, a combination of weight loss and exercise improve HDL function.27 Control blood glucose levels since both prediabetes and diabetes cause a loss of HDL functionality. In obese people 7 to 15% weight loss can help the lower elevated blood sugar. See the endocrine and diabetes section of this blog for more information on how to reverse prediabetes and type 2 diabetes.
Dietary factors that improve HDL function.
Choose to eat a Mediterranean-like, plant-based diet that includes legumes and monounsaturated fats. Eliminate trans and saturated fats. A plant-based diet with monounsaturated fats (olives, avocadoes, and almonds) improves HDL functionality. 28 It is better to eat the whole nuts, avocados, and olives than to use refined oil. However, cold-pressed extra virgin olive oil improves HDL functionality.29
Anthocyanins from whole blue, red, or purple fruits, and lycopene from tomatoes may improve HDL functionality.30
Reduce inflammation.
Since dysfunctional HDL are pro-inflammatory, eating a predominately whole plant food diet, getting enough sleep, regularity for sleep times and meals (to align circadian rhythms), and paying careful attention to gut health will reduce the inflammatory effects of dysfunctional HDLs. The diseases that cause dysfunctional HDL are pro-inflammatory. There is considerable evidence that anti-inflammatory strategies help to control and in some cases reverse them.
Summary:
Do you know your risk factors for coronary artery disease? Although your HDL number is important, it can fool you into false security if you have any condition that renders HDLs dysfunctional. Healthful lifestyle strategies can help to prevent and reverse atherosclerosis. Please work with your doctor and health care team to correct any unhealthy lifestyle practices and get any needed treatments.
Wildwood Lifestyle Center and Wildwood Lifestyle Outpatient Clinic specializes in reversing prediabetes and type 2 diabetes, lowering insulin requirements for type 1 diabetes, natural weight loss, reversing metabolic syndrome, non-alcoholic fatty liver diseases, early stage chronic kidney disease, and so much more.
Our outpatient clinic serves Chattanooga and northwest Georgia. Telemedicine consults are available to Georgian residents once they have been seen by one of our health providers.
Additional Information:
See this link https://wildwoodhealth.com/category/hypertension/ for articles on natural remedies for hypertension.
Visit the link https://wildwoodhealth.com/category/obesity-weight-loss/ for articles on obesity and weight loss.
For diabetes, visit the link https://wildwoodhealth.com/category/diabetes-endocrine-health/ for helpful strategies on reversing prediabetes and type 2 diabetes.
© 2024, Wildwood Sanitarium. All rights reserved.
Disclaimer: The information in this article is educational and general in nature. Neither Wildwood Lifestyle Center, its entities, nor author intend this article as a substitute for medical diagnosis, counsel, or treatment by a qualified health professional.
Sources
- Esin Eren. High Density Lipoprotein and its Dysfunction. Open Biochem J. 2012; 6: 78–93.↩
- Ragbir S. Dysfunctional high-density lipoprotein and atherosclerosis. Curr Atheroscler Rep. 2010 Sep; 12(5):343-8.↩
- University of Bonn. “How ‘good cholesterol’ stops inflammation.”ScienceDaily, 9 December 2013. www.sciencedaily.com/releases/2013/12/131209105240.htm.↩
- Riwanto M. High density lipoproteins and endothelial functions: mechanistic insights and alterations in cardiovascular disease. J Lipid Res. 2013 Dec; 54(12):3227-43.↩
- Riwanto M. High density lipoproteins and endothelial functions: mechanistic insights and alterations in cardiovascular disease. J Lipid Res. 2013 Dec; 54(12):3227-43.↩
- Ertek S. High-density lipoprotein (HDL) Dysfunction and Future of HDL. Curr Vasc Pharmacol. 2017 Nov 16.↩
- Helsingin Yliopisto (University of Helsinki). “Low HDL-cholesterol: Not quantity, but quality.” ScienceDaily, 30 April 2013. www.sciencedaily.com/releases/2013/04/130430091629.htm.↩
- University of Maryland Medical Center. “Has HDL, the ‘good’ cholesterol, been hyped?” ScienceDaily. ScienceDaily, 10 May 2016. www.sciencedaily.com/releases/2016/05/160510165110.htm.↩
- HDL cholesterol: How to Boost Your Good Cholesterol. www.mayoclinic.org/hdl-cholesterol/↩
- HDL cholesterol: How to Boost Your Good Cholesterol. www.mayoclinic.org/hdl-cholesterol/↩
- HDL cholesterol: How to Boost Your Good Cholesterol. www.mayoclinic.org/hdl-cholesterol/↩
- Farbstein D. HDL dysfunction in diabetes: causes and possible treatments. Expert Rev Cardiovasc Ther. 2012 Mar; 10(3): 353–361.↩
- Enas. Dysfunctional HDL. www.cadiresearch.org/topic/cholesterol/dysfunctional-hdl↩
- Kontush A. Functionally defective high-density lipoprotein: a new therapeutic target at the crossroads of dyslipidemia, inflammation, and atherosclerosis.↩
- Paoletti R. Review: Inflammation in atherosclerosis and implications for therapy. Circulation. 2004 Jun 15; 109(23 Suppl 1):III20-6.↩
- Katsiki N. High-density lipoprotein, vascular risk, cancer and infection: a case of quantity and quality? Curr Med Chem. 2014; 21(25):2917-26.↩
- Esin Eren. High Density Lipoprotein and its Dysfunction. Open Biochem J. 2012; 6: 78–93↩
- Halvorsen B. Determination of lipid oxidation products in vegetable oils and marine omega-3 supplements. Food Nutr Res. 2011; 55: 10.3402/fnr.v55i0.5792.↩
- He BM. Effects of cigarette smoking on HDL quantity and function: Implications for atherosclerosis. J Cell Biochem. 2013 Jul 15.↩
- Nicholls S. Consumption of Saturated Fat Impairs the Anti-Inflammatory Properties of High-Density Lipoproteins and Endothelial Function. www.sciencedirect.com/science/article/pii/S073510970601338↩
- Serban C. Dysfunctional HDL: the journey from savior to slayer (2014) Dysfunctional HDL: the journey from savior to slayer, Clinical Lipidology, 9:1, 49-59. 2014.↩
- Homocysteine and MTHFR Mutations | Circulation. circ.ahajournals.org/content/111/19/e289↩
- University of California, Los Angeles (UCLA), Health Sciences. “Jekyll into Hyde: Breathing auto emissions turns HDL cholesterol from ‘good’ to ‘bad’.” ScienceDaily. ScienceDaily, 15 May 2013. www.sciencedaily.com/releases/2013/05/130515174027.htm↩
- Association between circadian preference and blood lipid levels using a 1:1:1 propensity score matching analysis. J Clin Lipidol. 2019 Jul-Aug;13(4):645-653.e2. doi: 10.1016/j.jacl.2019.04.007.↩
- Stanton K. Moderate‐ and High‐Intensity Exercise Improves Lipoprotein Profile and Cholesterol Efflux Capacity in Healthy Young Men. Journal of the American Heart Association. June 21, 2022
Vol 11, Issue12. https://www.ahajournals.org/doi/10.1161/JAHA.121.023386 ↩ - Jomard J. High Density Lipoproteins: Metabolism, Function, and Therapeutic Potential. Front. Cardiovasc. Med., 31 March 2020. ↩
- Khan A. Weight Loss and Exercise Alter the High-Density Lipoprotein Lipidome and Improve High-Density Lipoprotein Functionality in Metabolic Syndrome. Arteriosclerosis, Thrombosis, and Vascular Physiology. vol. 38:2 2018;38:438–447. https://www.ahajournals.org/doi/10.1161/ATVBAHA.117.310212↩
- Ronca A. Effects of a dietary intervention with Mediterranean vs lacto-ovo vegetarian diets on HDL function: Results from the CARDIVEG study. Nutrition, Metabolism, and Cardiovascular Disease. Volume 33, Issue 3, March 2023, Pages 651-658↩
- Standler J. Front Nutr. 2021; 8: 761170. Dietary Strategies to Improve Cardiovascular Health: Focus on Increasing High-Density Lipoprotein Functionality↩
- Bardagjy, A.S. Relationship Between HDL Functional Characteristics and Cardiovascular Health and Potential Impact of Dietary Patterns: A Narrative Review. Nutrients. 2019 Jun; 11(6): 1231.↩